Building eConsult Programs Aligned to Quality Initiatives for More Effective Value-Based Care
As primary care providers and health systems transition from traditional fee-for-service models to value-based care (VBC), eConsults are a scalable,…
Managing patients with multiple chronic conditions (MCCs) is a major challenge for primary care providers (PCPs). Nearly 30% of Americans and 4 in 5 Medicare beneficiaries fall into this category1. The complexity of overlapping conditions and lack of integrated care significantly increases the risk for these patients and brings particular challenges to their management2,3.
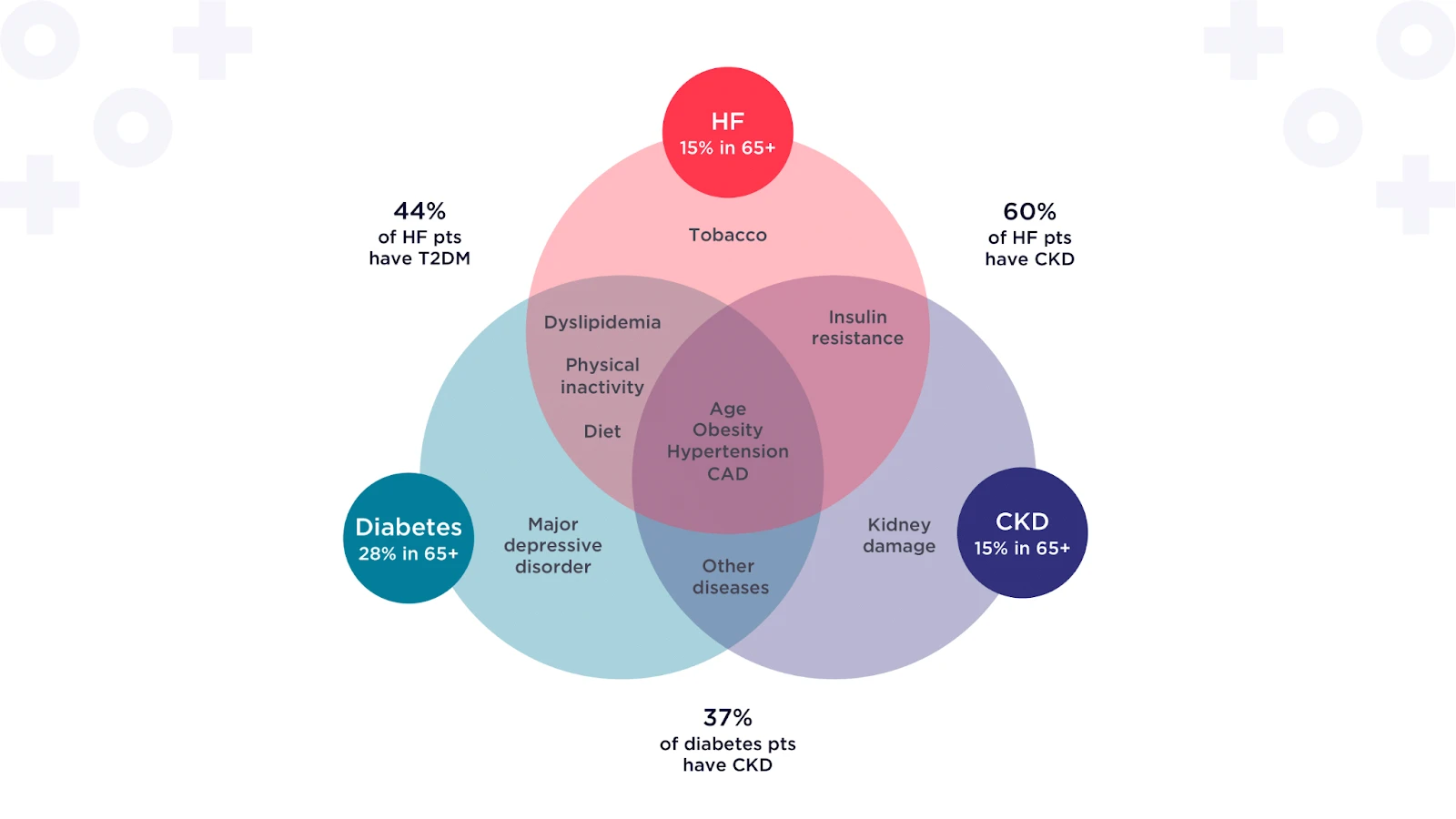
There is significant overlap across three of the most common multiple chronic conditions1, 4: Diabetes, Chronic Kidney Disease (CKD), and Heart Failure (HF). Management of the cardio-renal-metabolic system (see graphic) requires multiple specialists to focus on the heart, kidneys, and endocrine system.
Overlapping risk factors increase cardio-renal-metabolic risk5-9
An unmet need; multispecialty care for cardio-renal-metabolic disease
The current delivery models are focused on sub-specialization, where each specialty is considered a separate entity to manage a specific disease. However, RubiconMD understands that there is a complex interplay across conditions. Our eConsult+ platform provides the first step in leveraging more coordinated, integrated care delivery models.
Reasons to pursue innovative tech solutions to optimize MCC care:
Providing high-quality multispecialty support for clinicians with MCC patients
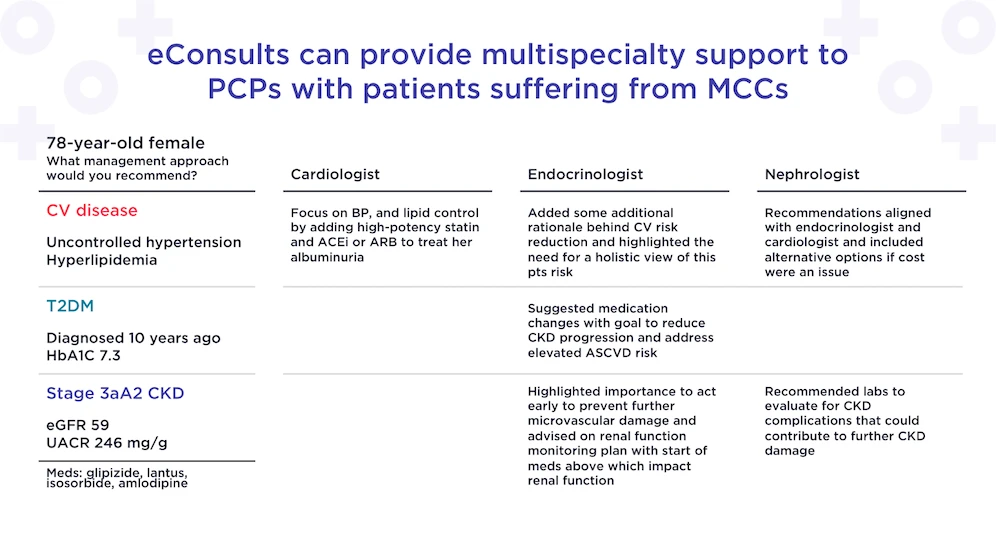
The Cardiologist, Endocrinologist, and Nephrologist are available on the RubiconMD eConsult+ platform, all working to support the PCP. Here, we can see how each specialist addresses and recognizes the complex interplay of the various chronic conditions and recommends appropriate options acknowledging the interconnectedness of the other conditions.
This could not be efficiently accomplished in a traditional care setting as the patient would actually need to be referred to three different specialists, with the added risk of incomplete referral follow-throughs. Additionally, the lack of communication and documentation sharing between different specialists often leads to siloed care resulting in therapeutic inertia and conflicting recommendations10. Finally, communication between the specialists and the PCP is frequently fragmented which may limit opportunities to improve the management of patients with MCCs in primary care.
RubiconMD’s eConsult+
Learn more or schedule a demo today.
Sources:
As primary care providers and health systems transition from traditional fee-for-service models to value-based care (VBC), eConsults are a scalable,…
Access to specialty care shouldn’t depend on your zip code, insurance type, or income level—but for Medicaid patients, it often…
In recent years, eConsults have emerged as an impactful tool for health plans to increase value and lower specialty care…

Explore real examples of specialty care eConsults providing efficient and effective support for medication review and reconciliation.